OHIP and Medicaid
Funding problems abound in both the Canadian and American systems for which governments pay the bills. These systems are very popular with the public - politicians don’t dare mess with them 🤨
Medicaid Debate
As I read this article, I couldn’t help but compare the Medicaid system to OHIP and Health Canada 🧐
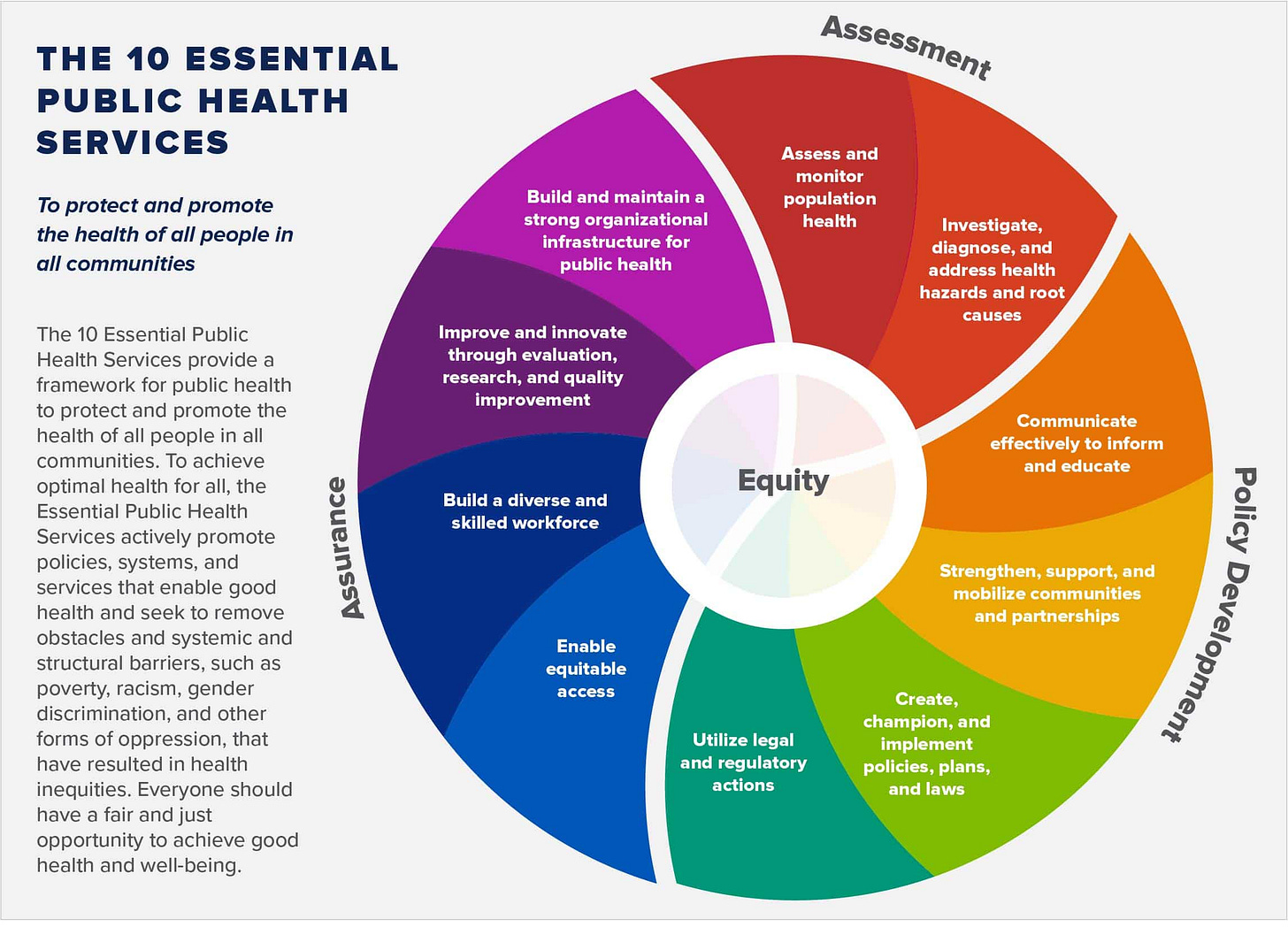
Both systems suffer from excessive government intervention and oversight. What’s even worse, however, is that the World Health Organization looms increasingly in the background - an ominous spectre that lays the heavy hand of additional bureaucratic oversight that surely carries a hefty price tag too.
At the bottom of this bureaucratic authority pyramid is you, me and our loved ones.
Our voice for change to these systems is very weak. It is muted by political roadblocks, entrenched special interests and hidden bureaucratic tripwires that have proven insurmountable to our best efforts.
GROK helps
Below is a SWOT analysis comparing the American Medicaid system and the Canadian Ontario Health Insurance Plan (OHIP) system, focusing on their strengths, weaknesses, opportunities, and threats. The analysis is structured to highlight key aspects of each system while drawing contrasts where relevant.
American Medicaid System
Strengths:
Targeted Coverage: Provides healthcare to low-income individuals, children, pregnant women, elderly, and disabled populations, covering over 80 million Americans (as of recent data).
Federal-State Partnership: Flexibility allows states to tailor programs to local needs, with federal funding covering 50-90% of costs depending on state wealth.
Broad Services: Includes hospital care, doctor visits, long-term care, and preventive services, with some states expanding to dental and vision.
ACA Expansion: The Affordable Care Act enabled states to expand eligibility, reducing uninsured rates significantly in participating states.
Weaknesses:
Inconsistent Coverage: Eligibility and benefits vary widely by state, creating disparities (e.g., expansion states cover more adults than non-expansion states).
Administrative Complexity: State-specific rules and bureaucracy can confuse beneficiaries and providers, leading to delays or denials.
Provider Participation: Low reimbursement rates discourage some doctors from accepting Medicaid patients, limiting access to care.
Funding Strains: High costs strain state budgets, especially during economic downturns, risking cuts to benefits or eligibility.
Opportunities:
Technology Integration: Telehealth and digital health records could improve access and efficiency, especially in rural areas.
Policy Reforms: Standardizing benefits or increasing federal funding could reduce disparities and improve care quality.
Value-Based Care: Shifting to outcome-based payment models could incentivize better health outcomes and cost control.
Public Health Focus: Expanded preventive care and social determinants of health (e.g., housing, nutrition) could reduce long-term costs.
Threats:
Political Instability: Changes in federal or state leadership can lead to funding cuts, eligibility restrictions, or program restructuring.
Economic Downturns: Recessions increase enrollment while reducing state revenues, straining budgets.
Aging Population: Rising demand for long-term care (e.g., nursing homes) could overwhelm budgets without reform.
Legal Challenges: Ongoing lawsuits over ACA or Medicaid expansion could disrupt coverage for millions.
Canadian OHIP System
Strengths:
Universal Coverage: Covers all Ontario residents for medically necessary hospital and physician services, ensuring broad access.
Single-Payer Efficiency: Centralized administration reduces overhead costs compared to private insurance models (administrative costs ~1-2% vs. 12-18% in U.S. private systems).
Equitable Access: Eliminates financial barriers for covered services, reducing health disparities across income levels.
Portability: Benefits are transferable across Canada, supporting mobility within the country.
Weaknesses:
Limited Scope: Does not cover prescription drugs (outside hospitals), dental, vision, or allied health services (e.g., physiotherapy), forcing reliance on private insurance or out-of-pocket payments.
Wait Times: High demand for non-emergency procedures (e.g., MRIs, elective surgeries) can lead to delays, sometimes months.
Provider Shortages: Rural and remote areas face shortages of doctors and specialists, limiting access.
Funding Pressures: Relies on provincial taxes, which can strain budgets during economic slowdowns.
Opportunities:
Expanded Coverage: Including pharmaceuticals, mental health, or dental care could address gaps and improve overall health outcomes.
Digital Health: Telemedicine and AI-driven diagnostics could reduce wait times and improve access in underserved areas.
Workforce Investment: Training and incentivizing more healthcare professionals could address shortages, especially in rural regions.
Preventive Care: Greater focus on public health initiatives could reduce demand for acute care, easing system pressures.
Threats:
Aging Population: Increased demand for chronic disease management and long-term care could strain resources.
Federal-Provincial Tensions: Disputes over federal health transfers may limit Ontario’s ability to fund OHIP adequately.
Private Care Push: Growing frustration with wait times fuels calls for private healthcare, which could undermine the public system.
Economic Volatility: Recessions or rising costs (e.g., new treatments) could force budget cuts or tax increases, risking public support.
Comparative Insights
Coverage Scope: Medicaid offers broader benefits (e.g., long-term care, some dental/vision) but is means-tested, while OHIP is universal but excludes key services like drugs and dental.
Access and Equity: OHIP ensures equitable access to covered services, while Medicaid’s state variability creates inequities. However, OHIP’s wait times and provider shortages can limit timely access.
Funding and Stability: Both systems face economic and political risks, but Medicaid’s federal-state split adds complexity, while OHIP’s single-payer model simplifies administration but relies heavily on provincial budgets.
Future Challenges: Both must address aging populations and rising healthcare costs. Medicaid could benefit from standardization, while OHIP needs to tackle wait times and coverage gaps.
If you’d like a deeper dive into specific aspects (e.g., data on wait times, reimbursement rates, or policy proposals), let me know, and I can search for real-time information or analyze relevant sources!
Bias
GROK does not provide a Libertarian LESS GOVERNMENT perspective. I would have liked to see how reducing the monopoly hold of those systems on the public would benefit from more competition - a greater range of choices based on a variety of metrics that reward good health and lifestyle behaviours offered at competitive prices. These is a reason why 60% of American (200 million citizens) suffer from metabolic syndrome and this has little to do with bad family genes.
GROK, like most AI LLM platforms, reflects the views of the majority of content writers whose published documents have been used to train GROK.
The vast majority of that digital content supports the idea that governments have an important and legitimate role in society to protect people from their own worst health habits. 😐
Individual Freedom and Personal Responsibility are virtues that are missing in GROK’s analysis 😡
This omission continues to reinforce that prevailing attitude that more BIG GOVERNMENT is more desirable than these virtues